Celiac Disease: Barriers to Diagnosis
Published April, 2021
If getting your celiac disease diagnosis is taking (or took) a long time, you are not alone. The journey to diagnosis can take a while for individuals with celiac disease. We spoke to some experts who treat celiac disease patients to better understand some of the barriers that can interfere with a prompt diagnosis.
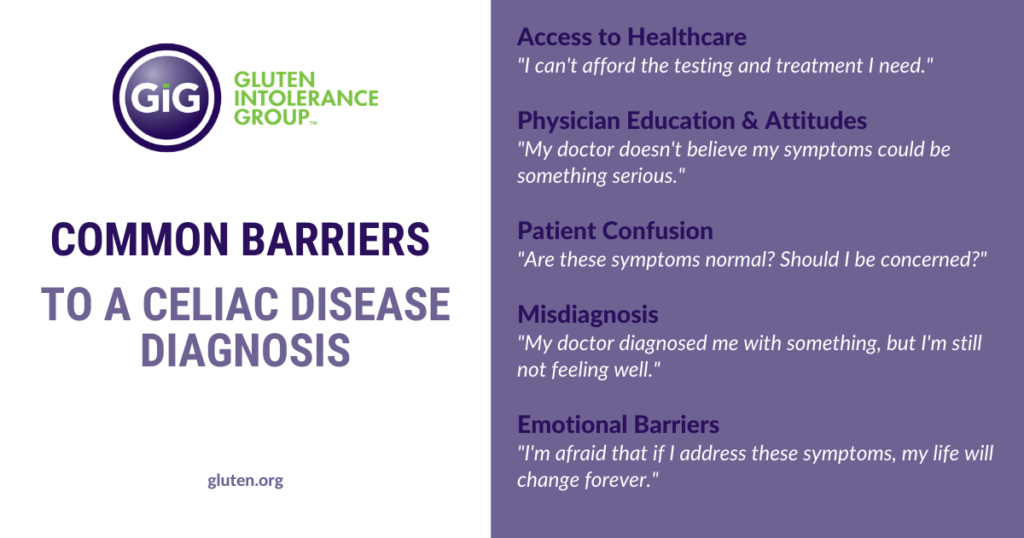
Patient Confusion/Attitudes
When you’re not feeling well, looking at your symptoms is a typical way to try to figure out what’s wrong. Dr. Stephen Wangen, ND, founder and medical director at IBS Treatment Center, points to the huge number of symptoms that can occur in celiac disease and says that even though awareness has grown in the past 20 years, it can still be confusing.
According to the University of Chicago’s Celiac Disease Center, there are over 200 symptoms that can be associated with celiac disease. Symptoms can vary depending on a number of factors, like your age or how long you’ve been undiagnosed and untreated. Talk about a lot to keep in mind!
Speaking of symptoms, Wangen says another barrier to diagnosis that he sees in his practice is that celiac disease doesn’t have to include diarrhea. Celiac disease doesn’t even have to include any digestive symptoms at all.
Another barrier could be an attitude some people have about what it means to be healthy.
“One huge issue is that our acceptance of what is normal health underestimates our capacity for excellent health,” says Wangen. “We assume that people should have less than perfect health. We assume that people with perfect health are unusual and not the norm.”
Some stomach upset? Oh, it’s probably just stress. Canker sores now and then? Well, that’s been happening since childhood so it’s just what happens. Sound familiar?
Feeling unwell isn’t normal – it is a sign that something in your body is out of balance or damaged. In the case of untreated celiac disease, what you’re feeling could be your body responding to the damage that gluten is causing. But you may not be getting the message because you don’t yet understand the signs.
Physician Education/Attitudes
You’re not the only one who might not think of celiac disease when considering the symptoms that you’re experiencing. Your healthcare provider may not, either.
“I think that knowledge is growing among many healthcare centers to more consistently screen for (celiac disease),” says Alyse Bedell, PhD GI, a Health Psychologist and Assistant Professor of Psychiatry & Behavioral Neuroscience at The University of Chicago. “However, if a person has access to a hospital system or medical provider that doesn’t consistently have that on their radar, this could result in significant delays in receiving the diagnosis.”
Red flags that could signal to a doctor that some testing might be in order include your family having a history of celiac disease or related auto-immune disorders including those that affect the gut like Crohn’s disease, for example. Even if members of your family are simply sensitive to gluten, that’s a sign that should not be ignored.
Your next step should be talking to your healthcare provider about getting tested. If your healthcare provider isn’t thinking about celiac disease, or your symptoms don’t seem like the ones they’ve learned about, they may not pursue testing.
What if your healthcare provider doesn’t listen to you or dismisses what you are saying when you describe the different symptoms you’re feeling?
“Sometimes people have negative interactions with healthcare providers and end up feeling dismissed or like their symptoms aren’t real,” says Bedell. “These kinds of experiences can be hard to bounce back from. It can contribute to stigma, depression, anxiety, and can impact whether a person even continues to seek medical treatment.”
Taking charge of your health and healthcare experience can be hard, but it is an important step to getting to the right provider who hears you. What you’re experiencing is not uncommon – and it’s not you.
Lola O’Rourke, MS, RDN, GIG’s Education Coordinator, says that being informed and asking questions about celiac screening is a step toward helping a physician become more aware.
“On a broader level, increasing awareness of celiac disease and gluten-related disorders in the general population, as well as within medical communities, can help address this barrier,” says O’Rourke.
Misdiagnosis (Mistaken for Something Else)
The many symptoms that can be associated with celiac disease creates more problems when it comes to diagnosis, including possibly getting the wrong diagnosis.
According to Bedell, some of the symptoms of celiac disease are “non-specific” and might look a lot like symptoms of other disorders.
“For example, digestive symptoms like diarrhea or abdominal pain are common in irritable bowel syndrome (IBS), a different gastrointestinal diagnosis that is very commonly seen in GI departments and primary care,” she says. “Symptoms like fatigue and weight loss can be seen in mental health conditions like a depressive disorder, which is another common condition.”
Being misdiagnosed can be costly in more ways than one.
“Some people probably spend significant time, energy, and money trying to manage their symptoms and see doctors and have tests to figure out the cause of the problem,” says Bedell, and these experiences can take their toll.
Emotional Barriers
Depending on where you are in your journey to figure out why you are unwell, there may be some internal or emotional factors that are keeping you from getting a proper diagnosis.
“Sometimes patients are hesitant to seek medical care and receive testing. We see this in lots of medical conditions and call it ‘avoidance,” says Bedell. “It’s really a sometimes-unconscious attempt to protect oneself, such as protecting oneself from the stress and anxiety of receiving a diagnosis. The avoidance is coming from a genuine place, but it isn’t actually helping to protect a person and actually might be causing more harm and suffering.”
Bedell advises that if someone suspects that they have celiac disease and are afraid to seek help, they should find a support system to help them through that process.
“It could be a friend or family member that can be an accountability partner, or maybe a therapist who can help them address some of their anxiety and provide strategies and support as they go through that process,” she says. “Remember that, for better or worse, you getting tested is not what determines whether you have celiac disease. It’s either there or it’s not. But your ability to get tested and to identify if you have it will allow you to make a plan to address it.”
Bedell adds that receiving a diagnosis of celiac disease might come with relief, but it might also come with a lot of mixed emotions including grief, loss, anxiety, and fear. If you have the right support, she says, there is a path forward through those mixed feelings, even if its alongside those feelings.
O’Rourke says that in addition to friends and family, another way to get through the fear of diagnosis is peer support. GIG Support Groups are free to join, and members can help before, during, and after diagnosis.
Limited Access to Quality Healthcare
Another potential barrier could be financial or a lack of medical insurance that keeps some people from even seeking help at all. According to the CDC, in 2019, 32.8 million people in the United States under the age of 65 were uninsured, and the most common reason was that they could not afford the medical insurance.
Over time, a person with undiagnosed and untreated celiac disease can get sicker. The physical and emotional effects of untreated celiac disease can build up, potentially creating a more extreme health situation that becomes even more expensive in the long run.
As you can see, there are a lot of reasons why someone might not get a proper diagnosis. When it comes to getting a proper diagnosis and treatment for celiac disease, more needs to be done to ensure that everyone has access to quality healthcare. Educating yourself about celiac disease and finding resources and support are good places to start. Check out the Getting Started section on our website for more information.
